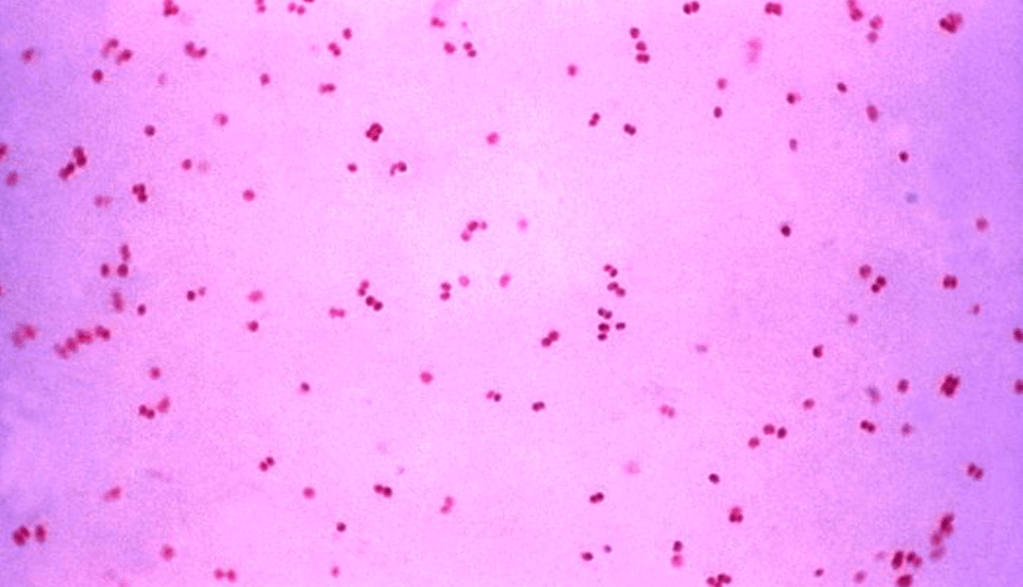
Sexually Transmitted Diseases (STDs) are some of the most widely spread communicable diseases in the United States. Gonorrhea alone is the second most commonly reported disease in the US according to the CDC. Gonorrhea is caused by the bacteria Neisseria gonorrhoeae. This STD infects both women and men through sexual contact and can also spread from pregnant women to their babies through vaginal birth. One of the reasons this STD in particular is so readily spread is due to the fact that many infected people are asymptomatic. In addition to the ease of spread and potential lack of awareness of one’s own status, recently fighting gonorrhea has seen challenges with antibiotic resistance and increasing prevalence.
Rates of gonorrhea in the US have risen over 126% from 2007-2018 according to the US News and World Report. Unfortunately, these statistics are not uncommon for STDs–nearly all of them are statistically on the rise. Perhaps most interesting in the data gathered from the above time period is the gender breakdown for gonorrhea though. For male patients gonorrhea diagnosis increased by 326%, but for female patients it only increased by 47%. While an increase at any rate may be cause for concern, the stark difference between the rates was striking. Furthermore, this discrepancy factors into the change from what in 2007 was a near 50/50 distribution of STD diagnoses between male and female patients to a 61/39 distribution in 2018 (the 61% corresponding to male cases). The cause for this increased prevalence in the US is hard to pin point. Is it that more people are taking control of their health and getting tested? Are people practicing less safe sex? Either way, increased prevalence leads to greater risk of transmission.
As rates of transmission appear to increase, antibiotic resistance complicates gonorrhea treatment. According to a study discussed by MedicalXpress this month, N. gonorrhoeae is highly adaptable and adapted over time to human cells. It’s variable nature has been integral in developing antibiotic resistance. Gonorrhea has shown resistance to every antibiotic used to treat it thus far. In promising news though, the researchers of this study believe they have data to support two viable non-antibiotic drugs that could be repurposed to act to prevent and cure gonorrhea in female patients. These drugs, methyldopa and carbamazepine, are currently used to treat hypertension in pregnant women and epilepsy respectively. Both work by competing with bacteria to bind CR3 though, and these researchers believe that may be the key in preventing and curing gonorrhea in female patients. These drugs will still need to be tested and vetted extensively before being prescribed commercially. Even if we speak as optimistically as possible and say these drugs will cure and prevent female patient infection, we still have to worry about the extremely high and increasing rate of infection in male patients. It is a promising breakthrough, but just like in so many other sectors, so much more must be done in researching viable alternative to antibiotic treatment.