Be yourself; Everyone else is already taken.
— Oscar Wilde.
This is the first post on my new blog. I’m just getting this new blog going, so stay tuned for more. Subscribe below to get notified when I post new updates.
Be yourself; Everyone else is already taken.
— Oscar Wilde.
This is the first post on my new blog. I’m just getting this new blog going, so stay tuned for more. Subscribe below to get notified when I post new updates.
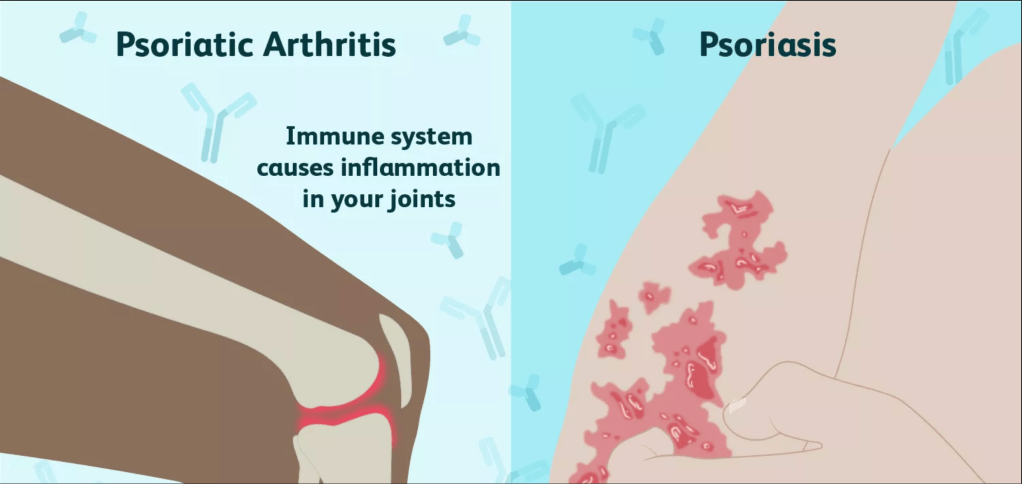
Secukinumab, the drug commercially marketed as Cosentyx, is a monoclonal antibody medication frequently used by sufferers of plaque psoriasis and psoriatic arthritis. Plaque psoriasis is an autoimmune disease affecting the skin that results in raised reddish patches that are covered with whitish buildup of dead skin cells that are often painful and/or itchy. These patches are usually present on the elbows, knees, scalp, or lower back; but they can show up anywhere. T cells and neutrophils in a patient attack healthy skin cells as if they were fighting a wound or infection. These over-acting skin cells can create inflammation in the joints by producing too many new skin cells where there isn’t a need, a condition referred to as psoriatic arthritis. The arthritic condition typically develops after the patches related to psoriasis have appeared, but not always.
Monoclonal antibody drugs like Cosentyx were an answer the experimental issue of our immune systems responding to all of the epitopes of an antigen, resulting in polyclonal antibodies. This is a problem primarily because the antiserum is then different in each time. Monoclonal antibodies are produced by a clone of one type of B cell. Therefore, they attack the same epitope of an antigen. Cosentyx acts as an anti-inflammatory by targeting the cytokine IL-17A, one of the molecules believed to directly affect the inflammation associated with psoriatic disorders. Cosentyx is administered to the patient via injection once a month after the initial weekly shots for four weeks.
Side effects associated with Cosentyx include:
Cosentyx works as an anti-inflammatory. This means that it inhibits the innate immune system’s natural responses. While this is useful for the autoimmune condition of psoriasis in that it prevents excessive inflammation in the skin and joints, it also prevents the immune system from attacking actual infections. This mechanism is likely why patients see an increase in upper respiratory tract infections, rhinitis, etc. There are also several drug interactions and adverse reactions to be aware of. In addition to an increased risk of infection by suppressing immune response, the drug also saw many patients in clinical trials experience inflammatory bowl disease and exacerbation of ulcerative colitis. These are inflammatory conditions as well, so it makes sense that Cosentyx would exacerbate them. It is advised that the drug not be administered to patients with an active tuberculosis (TB) infection, and that those with latent TB should be treated prior to starting Cosentyx. The body relies on the immune system to help fight the infection, and Cosentyx negatively impact the innate immune response.
So, is this monoclonal antibody drug a god-send for sufferers like Kim Kardashian West and Art Garfunkel (I know, what a pair)? The answer is unclear. It has given relief to many suffering from psoriasis, but it is important to also consider the side effects of inhibiting IL-17A from binding to the body’s IL-17 receptor–effectively diminishing the innate inflammatory response. What is clear though is that the monoclonal antibody response has been a true breakthrough in developing drug therapy for autoimmune diseases like psoriasis. The hope is of course that research will continue in pursuit of even better drugs with less adverse effects.

Researchers have been scrambling to discover an effective way to track and test for 2019 novel coronavirus infections. These tests are critical in both assessing the spread and infectiousness of the virus as well as discerning what measures need to be taken moving forward. One of the biggest concerns at the moment is whether or not those who have been infected develop any immunity to the virus and how long that immunity may last. An article written last week in Time details the ongoing research into antibody testing and what immunity might look like for this virus. Given the news that some patients in China, Japan, and South Korea who were infected but seemingly recovered came back into the hospital and tested positive again, questions have arisen as to whether infected patients acquire effective immunity at all.
According to the article, most other coronavirus strains the antibodies produced give a person immunity for months or even years. It is too early to tell how long effective antibodies will remain in a patient’s system for this strain though. It is an extremely important question to answer though, as the immunity acquired to the virus has serious implications in the spread of the disease and the probability of reoccurring waves of infection across the globe. Experts have supposed that it is very unlikely that a patient would be reinfected soon after recovery, and suppose that the patients that were “re-infected” so quickly after recovering actually may have received false negative results and still been infected. They also suppose that an individual’s immunity to the virus may be related to the strength of the person’s immune system to start with. That is to say, the healthier and more robust the immune system is to start with, the better the immune response to this specific virus.
Just last week, the FDA approved the first COVID-19 blood test that tests for antibodies against the virus. In an article from BioSpace, the test is described as detecting IgM and IgG antibodies in the blood. IgM antibodies are generally detectable for several days after the initial infection. IgG antibodies are usually detectable further into the infectious course of the disease. Positive results for both IgM and IgG antibodies indicate the patient has either an active or recent infection with the virus. Only testing positive for IgM antibodies would indicate either the beginning the infection, before cross linking has taken place. If the presence of the IgG antibodies could be tested for independently, there would be more indication that a person had effective immunity. If a person has tested negative for an active infection by the RNA genome, but still has IgG antibodies, it would indicate immunity. The question still remains how long this immunity would last. These antibody tests will certainly be helpful in the continued work to fight this pandemic, but unfortunately it seems like we will have to wait longer to see the full scope of this virus and its effect on long-term public health.
Personalized medicine is a growing area in the medical field focused in an individualized approach to drug therapy based on an individual’s genetic makeup. T-Cell therapy is a technique currently gaining steam in the personalized medicine field, especially for those suffering from Mantle Cell Lymphoma. Mantle Cell Lymphoma is a cancer of the white blood cells often referred to as a type of non-Hodgkin’s Lymphoma. Essentially, this type of cancer causes your B Cell lymphocytes to multiply at an out-of-control rate resulting in tumor formation in lymph nodes and/or bone marrow. Because the cancer often isn’t discovered until it’s metastasized, the prognosis is typically bleak. Therefore, the breakthroughs being made with T-Cell therapy is quite exciting.

An article published this month in Lymphoma News Today discusses the proposal of a new CAR T-Cell therapy treatment called KTE-X19 to the FDA and EMA. CAR T-Cell therapy takes a patient’s T-Cells into the lab and genetically modifies them to recognize specific cancer molecules. KTE-X19 is designed to recognize a protein called CD19 found on the surface of some malignant B-Cells. A differentiating factor in this treatment from other T-Cell therapies targeting lymphomas is the ability to separate circulating tumor cells from immune cells. The results of the patient study done on this therapy are discussed in more detail in an article on the American Journal of Managed Care website. The study’s results showed that 85% of the entire study cohort achieved an objective response to the treatment. While that and a few other measures indicated promising success for the treatment, the study also found side effects. The article refers to the adverse side effects as grade 3 or higher with 91% of patients experiencing cytokine release syndrome, a condition characterized by multiple organ issues. Other common side-effects include infections and cytopenias, but according to the researchers all of the side effects were largely reversible.
While the side effects are certainly something to note, the results of this study and their proposal to national approving agencies is exciting for the field. Especially for a condition like MCL which typically only sees a ten-year survival rate between 5 and 10%, these drug therapies have great potential to change people’s lives. If continued success is seen in this therapy for lymphomas, doors may even be opened for further research on other cancers or auto-immune diseases. Long-term studies will still be needed of course to see 5 and 10 year outcomes. These glimmers of hope are always welcome in world of drug research, even if further fine tuning is still necessary.
So I love this meme, and it certainly describes my mood for the past two and a half weeks. With that being said, this is not at all fine. Graduation is postponed, all of our classes (including labs?!) are online, we can’t go out and do anything or see anyone, and to top it all off a killer virus is sweeping the globe. While listing all of that out feels exhausting at best, the day-to-day of it is what’s most grinding. It’s hard to focus on school or work when it feels like life will never go back to normal. But I know I don’t have to anyone that. Perhaps the only comforting thing in this debacle we’re currently calling life on earth is that we’re all going through the same thing.
Now that we’ve gotten through my emotions though, I’ll get to the real stuff. Upon the postponing of commencement and the decision to put classes online indefinitely, I decided it was time I pack my bags and fly home before all the flights were cancelled. So on to south Texas I went! But of course it wasn’t that easy. Only after one cancelled flight, 45 minutes on the phone with American Airlines, and several day-before connecting flight changes did I find myself at RDU waiting to board my flight. It was at this point in time that I saw something horrifying. Something that probably gives explanation as to how this virus is spreading like wildfire despite all of this “quarantining.” From my safe 6+ feet away seat I saw a woman go up to the airline counter wearing an N-95 surgical mask. She then proceeded to take off the mask to talk to the attendant and put the mask face down on the counter and then when finished speaking put the mask back on her face! Needless to say this made want to curl into a ball and be placed in a trash bag for the reminder of my flying experience. Please people, get it together.
Nonetheless, I did eventually make it home Monday afternoon just in time to jump into online classes. The time change has been a little tricky for remembering my classes, but other than that I’m very fortunate to be able to come home. I can’t lie though, this is stressful. Extremely stressful. I have an incredible newfound respect for our healthcare workers and grocery store clerks and other essential employees who are out everyday facing exposure. So yeah, this scary and inconvenient and extremely isolating. But being home has been a stress reducer–especially being home with my dog Daisy! Stay safe everyone, please please please follow the quarantine rules–as Dr. Cramer would say, wash your hands, don’t touch your face!

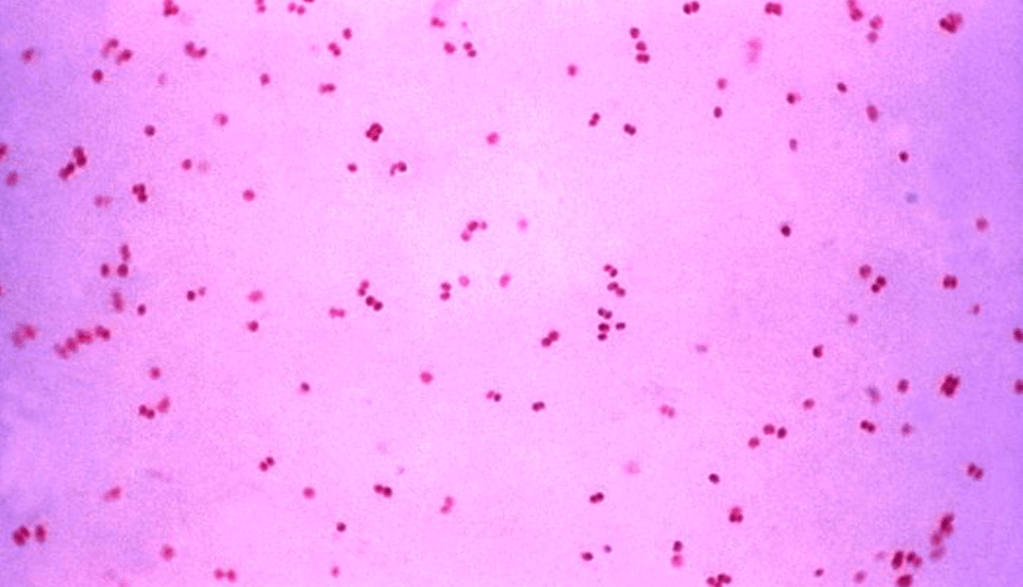
Sexually Transmitted Diseases (STDs) are some of the most widely spread communicable diseases in the United States. Gonorrhea alone is the second most commonly reported disease in the US according to the CDC. Gonorrhea is caused by the bacteria Neisseria gonorrhoeae. This STD infects both women and men through sexual contact and can also spread from pregnant women to their babies through vaginal birth. One of the reasons this STD in particular is so readily spread is due to the fact that many infected people are asymptomatic. In addition to the ease of spread and potential lack of awareness of one’s own status, recently fighting gonorrhea has seen challenges with antibiotic resistance and increasing prevalence.
Rates of gonorrhea in the US have risen over 126% from 2007-2018 according to the US News and World Report. Unfortunately, these statistics are not uncommon for STDs–nearly all of them are statistically on the rise. Perhaps most interesting in the data gathered from the above time period is the gender breakdown for gonorrhea though. For male patients gonorrhea diagnosis increased by 326%, but for female patients it only increased by 47%. While an increase at any rate may be cause for concern, the stark difference between the rates was striking. Furthermore, this discrepancy factors into the change from what in 2007 was a near 50/50 distribution of STD diagnoses between male and female patients to a 61/39 distribution in 2018 (the 61% corresponding to male cases). The cause for this increased prevalence in the US is hard to pin point. Is it that more people are taking control of their health and getting tested? Are people practicing less safe sex? Either way, increased prevalence leads to greater risk of transmission.
As rates of transmission appear to increase, antibiotic resistance complicates gonorrhea treatment. According to a study discussed by MedicalXpress this month, N. gonorrhoeae is highly adaptable and adapted over time to human cells. It’s variable nature has been integral in developing antibiotic resistance. Gonorrhea has shown resistance to every antibiotic used to treat it thus far. In promising news though, the researchers of this study believe they have data to support two viable non-antibiotic drugs that could be repurposed to act to prevent and cure gonorrhea in female patients. These drugs, methyldopa and carbamazepine, are currently used to treat hypertension in pregnant women and epilepsy respectively. Both work by competing with bacteria to bind CR3 though, and these researchers believe that may be the key in preventing and curing gonorrhea in female patients. These drugs will still need to be tested and vetted extensively before being prescribed commercially. Even if we speak as optimistically as possible and say these drugs will cure and prevent female patient infection, we still have to worry about the extremely high and increasing rate of infection in male patients. It is a promising breakthrough, but just like in so many other sectors, so much more must be done in researching viable alternative to antibiotic treatment.
Antibiotic resistance is a rapidly growing issue challenging medical professionals and our healthcare infrastructure at large. Resistance can occur naturally through spontaneous mutations in bacteria, but it is exasperated by misuse of antibiotics in humans and animals. A growing number of diseases are becoming increasingly resistant to antibiotics including pneumonia, tuberculosis, and salmonellosis. According to the World Health Organization (WHO), antibiotic resistance can influence health outcomes by increasing hospital stays and mortality rates. They recommend proper food handling and taking antibiotics as directed as ways an individual can help mitigate the growing public health crisis. One of the biggest issues with antibiotics is the emergence of “superbugs,” or diseases that have become resistant to the majority of currently used antibiotics.
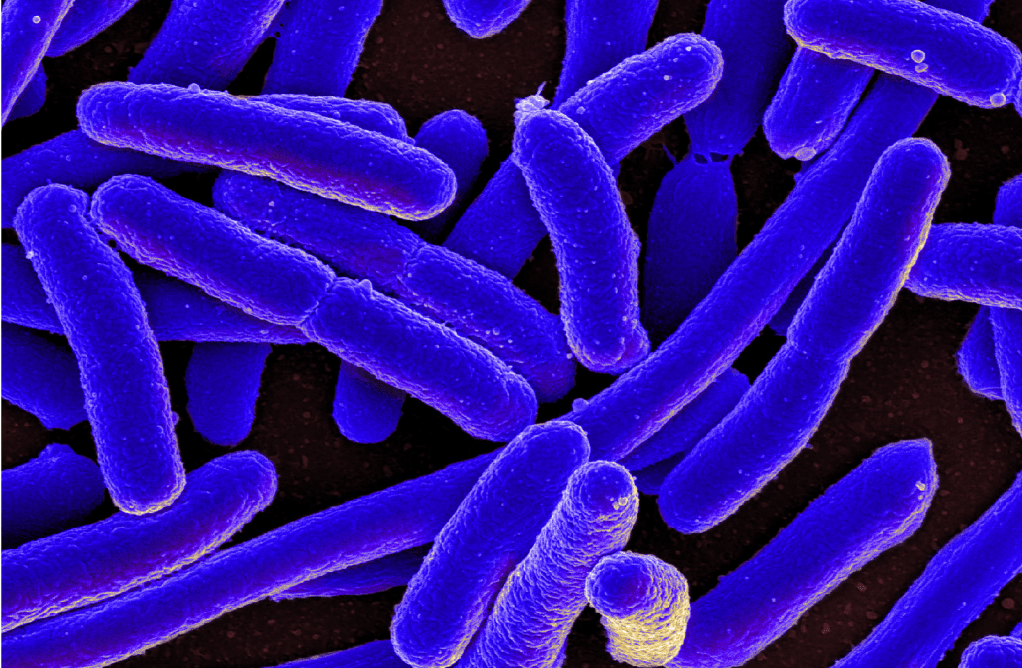
In an article from the Center for Infectious Disease Research and Policy at the University of Minnesota, researchers explore growing antibiotic resistance in pneumonia patients. The most notable finding from the study found that 22% of community-acquired pneumonia outpatients were resistant to antibiotics via statistics gathered US health insurance claims. The majority of the failed antibiotics were beta-lactam drugs. These adverse patient outcomes may spell disaster for elderly patients or immunocompromised patients. This gap in effective treatment highlights the need for increased funding for research in the field of antibiotic resistance.
Growing antibiotic resistance is also proving to be a challenge in cancer treatments. A Newsweek article from February details how chemotherapy treatment is being threatened by the emergence of superbugs. They estimate that 1 in 5 cancer patients will need antibiotics in during their treatment and 46% of UK doctors interviewed for the study said they believed drug-resistance will make chemotherapy useless in cancer treatment. Because chemotherapy weakens the immune system, it makes patients more susceptible to these emerging superbugs and without antibiotics they are at an extremely increased risk for adverse outcomes including death. Researchers quoted in the article call these finding a wake-up call in terms of the growing antibiotic resistance health crisis. I am inclined to agree as running out of viable antibiotics would likely create chaos. Many would die from bacterial infection before new effective drugs are approved if proper action is not taken now.
Poliomyelitis is a potentially deadly and/or extremely debilitating disease caused by the poliovirus. Because of widespread vaccination since the introduction of polio vaccine in 1955, the United States has been polio-free since 1979 according to the CDC. Despite low poliovirus incidence in the U.S. and other developed countries, many developing countries still face the threat. There two types of polio vaccine that provide immunity for the virus–inactivated polio vaccine (IPV) and oral polio vaccine. While both ultimately prevent the spread of polio, there are mitigating factors for each.
In the United States, IPV is the only vaccine series used for poliovirus since 2000. According to the CDC, children should receive four doses of the single-antigen vaccine at 2 months, 4 months, 6-18 months, and 4-6 years old. The vaccine is often contained in combination vaccines that lessen the amount of injections needed for children and infants, typically paired with DTAP, HepB, and or Hib. OPV, on the other hand, is used primarily in developing countries and is administered via droplets to the mouth. The Polio Global Eradication Initiative suggests that OPV is more efficient because it can be administered by volunteers. Additionally, they make the point that OPV has been declared Halal, which may be of consequence in many Muslim-majority countries still mitigating the poliovirus threat. OPV is also more cost-effective than IPV, making it more accessible for many developing countries. It is important to note though, that OPV requires several (even up to 10) doses to ensure immunity. Most concerning for me is that the exact number of doses needed is dependent on the child’s health and nutrition, creating a sort of guessing game that we may easily come out on the wrong side of.
Today, many in the U.S. think of polio as a thing of the past. Unfortunately though, according to Contagion Live, the 2018-2019 school year saw the number of children granted vaccine exemptions in public schools rise for the third consecutive year. This means that less and less children are getting the polio vaccine, and as world travel continues to become more prevalent, more opportunities arise for the poliovirus to strike again in the U.S. A response for this widespread vaccine-fear among parents has been combination vaccines. Contagion Live also reports new guidance from the CDC regarding a combination vaccine approved by the FDA in 2018 that protects against diphtheria, tetanus, hepatitis B, Haemophilus influenzae type B, and polio. The vaccine will become commercially available in 2021 and hopefully encourage higher immunity numbers among children.
In a January article from Newswise, concerns are raised about both IPV and OPV in the scope of truly eradicating polio. Children given OPV can apparently shed mutant polioviruses that cause paralysis while the manufacture of IPV uses wild viruses that pose a biosecurity threat. The WHO has called for the invention and manufacturing of safer polio vaccines in response to the apparent dangers of our current methods. Initial efforts have been using gamma radiation to inactivate the Sabin virus for a potential vaccine. While these results were promising both scientifically and economically, more will of course need to be done by way of testing before this supposedly safer vaccine is commercially available. Ultimately, while the work on a new vaccine is certainly critical, none of these great scientific advancements in terms of polio or any other virus will be truly significant if the anti-vax movement grows. It is imperative that our governments, schools, and hospitals strongly advocate for and educate on the subject of vaccines for the health and wellness of any generations to come.
Our microbiome has been at the forefront of medical disease research in recent years. Our microbiome is composed of trillions of bacterial cells and other microorganisms. A normal microbiota may contribute to proper digestion and a robust immune system. Imbalances in the microbiota, however, have been increasingly implicated in conditions like obesity, diabetes, and autism. In this particular article, I will discuss the recent studies into the microbiome’s influence on behavioral health. In a January study from Oxford University explored in New Atlas the idea that the gut microbiome has influence on our personality acquisition and behavior. While it doesn’t assert a direct connection, it does propose the idea of bi-directionality between gut microbiota and neuropsychiatric conditions. An interesting correlation was found between the diversity of the gut microbiome and increased sociability. Perhaps most interesting though is that study linked diversity of the microbiome to certain life choices like travel and diet.
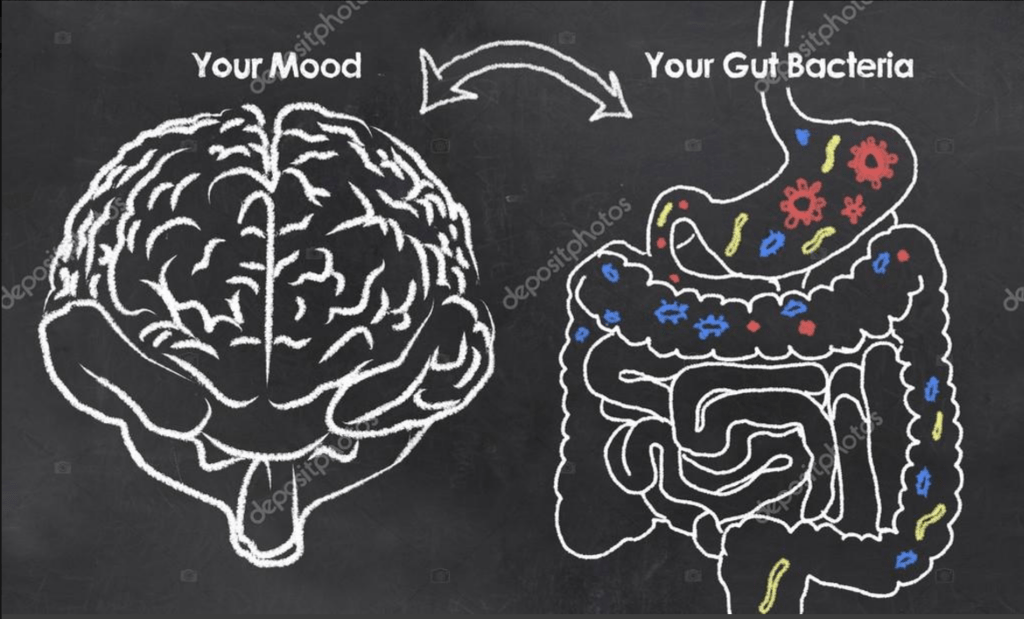
The link between gut microbiota and behavioral or mental health is quite fascinating. Given that research is so new though, many questions still remain. To what extent the microbiome plays a role in causing such psychological imbalances or abnormalities is yet to be seen. A convincing link, at least to me, has been made though between the microbiomes of the mentally well and those suffering from conditions like MDD. Perhaps the biggest question remaining though is how much influence we really have on our microbiota. The both studies point to diet as a potential major player in the microbiota, but diet is often heavily influenced by culture, socioeconomic status, and regional availability. The Oxford study specifically makes the point that modern-day living begets an insufficient diet. Is rectifying this modern diet and re-balancing the gut microbiota only a possibility for those who can afford to overhaul their pantry? I am sure many more studies are to come in this area, and as the science becomes more concrete, the social science will have much catching up to do.
Flu season is upon us once again. This time of year induces fear for many as the potentially lethal virus sweeps through universities, schools, and offices. Every year a new vaccine for the influenza virus must be created because new strains mutate every season through antigenic drift. This year’s flu is proving to be just as severe as the 2017-2018 season that was the deadliest in the past decade according to CNN reports discussed in this article from Time. Data released at the start of the new year reported in the article showed at least 6.4 million people in the United States have been diagnosed with influenza so far. Once more, 2900 people have died this season, 800 more than had been predicted by the CDC a week prior to releasing results. The flu has been particularly harsh in the past few years with deadly 2017-2018 season and the 2018-2019 season lasting 21 weeks. So what’s leading the charge this season in virulence? It may be related to this year’s vaccine.
Influenza has four different types of virus: A, B, C, and D. According to an article from Health, usually 75% of reported influenza cases are type A, but this season influenza B has been dominating. Influenza B is typically seen later in the flu season (mid to late spring), but symptoms mirror influenza A. However, influenza B infections can be more severe in children leading to more hospitalizations and deaths. Luckily, the flu vaccine protect against both influenza A and B. According to the CDC, this year’s vaccine will be quadrivalent with updates to some the protected strains for influenza A (H and N components) and the same strains protected from influenza B (B/Victoria and B/Yamagata components). The CDC projects that this year’s vaccine will be between 40-60% effective, but do not rule out significant antigenic drift.
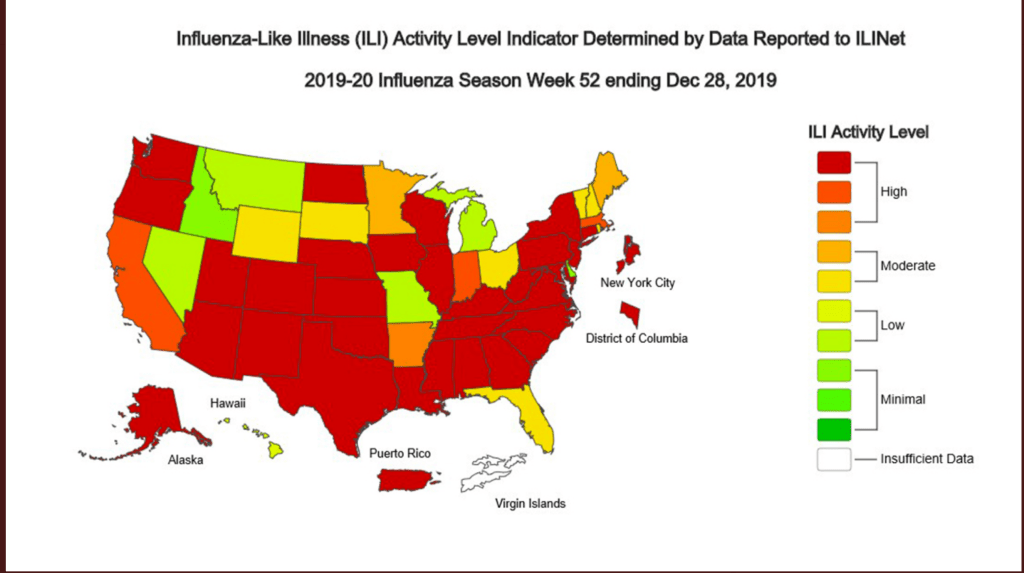
Despite the high risk of flu this season visualized in the graphic above, the flu vaccine is still the best bet in protecting against infection. Even for those who get the infection while having received the vaccine, the infection is less lethal and severe. While the vaccine is of course never 100% effective, some protection is always better than no protection. Especially with the influenza B strain spreading so rapidly this season, protecting vulnerable infants who are too young to receive the vaccine should be a top priority. The more adults who are vaccinated, particularly those who are frequently around children, the better protected the overall population will be.
Andrew Wakefield’s 1998 study published in The Lancet linked the attenuated vaccine for Measles, Mumps, and Rubella (also German Measles) to a gastrointestinal syndrome that was supposedly a trigger for autism. Despite great skepticism among the medical and scientific community upon the publishing of this work, and an expose published on the fraudulent nature of the study published in 2004, the article was not retracted until 2010. This article from WebMD outlines many of the issues with the study that led to retraction. Among them, a low sample size of only 12 patients who had been cherry-picked by Wakefield and his team for already being skeptical or opposed to the MMR vaccine. Furthermore, his results were immediately called into question by other doctors and scientists. Even for the 12 patients evaluated under this study, the results reported did not match the actual medical records. For example, only one of the children actually was diagnosed with regressive autism, despite the study claiming 9 out of the 12 had the diagnosis. Even beyond the fraudulent reporting, Wakefield never disclosed that he was paid by a U.K. lawyer, who was suing MMR vaccine makers, to the tune of nearly $700,000.
Despite the debunking of the link between the MMR vaccine and autism over 15 years ago, and the retraction of Wakefield’s article nearly 10 years ago, the legacy of Wakefield bringing skepticism and fear to the conversation about vaccines remains. This article from TIME outlines some of the ways immunization and disease rates have been affected in the 22 years since the Wakefield publishing and some ways to try to turn the clock back. Perhaps most alarmingly, in the U.S. where measles had been declared eliminated in 2000, a resurgence has been seen to the tune of over 2,000 cases. The article also highlights that even outside of the MMR vaccine specifically, Wakefield’s study has been influential in persuading individuals and importantly parents against vaccination in general. According to the TIME article 100-300 children under the age of five die from the flu, 85% of which were not vaccinated. The FDA has issued statements regarding their continued confidence in the MMR vaccine safety and utility to help combat this skepticism. In a 2019 statement, the agency made specific reference to large-scale studies that have demonstrated there is no link between autism and the vaccine.
Ultimately, for me, the skepticism surrounding vaccines in some circles is one of the most infuriating issues in public heath today. Not only is the argument against vaccines, and the MMR, vaccine in particular, completely lacking in terms of scientific evidence, but it also serves only to harm society at large. A common argument by anti-vaxers is that the individual should have the right to choose or not choose vaccination for themselves and their children. However, decreased vaccination rates damage herd immunity and put very young, very old, and immunocompromized individuals at great risk. Wakefield is of course not the sole reason for the anti-vaccination movement, but his study and its publication and media distribution had an undeniable effect on the modern conversation and attitude towards vaccines. To put it simply: the MMR vaccine is safe and effective. This blog is called “Victims of Virulence” for a reason–don’t be a victim if you don’t have to be one!